Nigerians are renowned for their unyielding resilience, unwavering determination, and extraordinary capacity to thrive in even the most challenging environments.
Their indomitable spirit, famously dubbed the ‘I can do’ mentality, is truly exceptional, and their ability to adapt and forge ahead even in the face of adversity is unparalleled.
With a remarkable talent for using obstacles as springboards for opportunities and not limitations, Nigerians have consistently demonstrated a unique ability to rise above highly difficult circumstances, making them a shining example of strength and fortitude in the face of adversity.
Despite the complex interplay of economic, social, and political factors affecting Nigerians’ quality of life, Nigeria has emerged as the happiest country in Africa and 102nd worldwide in the latest World Happiness Report.
Nigeria’s drop from 95th to 102nd in the happiness rankings suggests a subtle but significant downturn in the country’s wellbeing, mirroring the nation’s persistent struggles and transformations.
Nigerians are naturally adept at finding humour in life’s challenges and situations, with a remarkable ability to create joy and laughter even in the toughest of times.
However, despite our resilient spirit, there are cries for help going unnoticed, whispers of despair and desperation from those struggling to cope.
Amidst the strength and laughter, some individuals are silently suffocating under the weight of their struggles, turning to harmful substances and addictive behaviours as a misguided attempt to dull their pain and find temporary escape.
What is mental health?
Mental health crises are prevalent and real, and they cut across the strata of society, whether high or low, poor or rich.
According to Wikipedia, mental health is a state of well-being in which an individual realizes his or her abilities, can cope with life’s normal stresses, can work productively and fruitfully, and can contribute to his or her community.
Statistics
According to alarming statistics from the World Health Organization (WHO), approximately 25–30% of Nigeria’s population struggles with mental health issues, yet a staggering 90% of this affected group lacks access to professional help and resources.
According to a WHO report, the country has a significant gap in support and funding for mental wellness, with only 3% of the government’s healthcare budget dedicated to mental health services.
Types of mental health struggles, challenges
Mental health issues encompass a broad spectrum of conditions, and this list is by no means exhaustive.
Additionally, the severity and impact of mental health issues can vary greatly from person to person and even within the same individual over time.
Mental health issues include anxiety disorders (e.g., generalized anxiety, panic disorder, social anxiety), depressive disorders (e.g., major depressive disorder, postpartum depression), bipolar disorder, post-traumatic stress disorder (PTSD), and obsessive-compulsive disorder (OCD).
Also on the list are: schizophrenia, attention deficit hyperactivity disorder (ADHD), eating disorders (e.g., anorexia nervosa, bulimia nervosa), substance use disorders (e.g., drug addiction, alcoholism), and personality disorders (e.g., borderline personality disorder, narcissistic personality disorder).
The list also contains: trauma and stress-related disorders; dissociative disorders (e.g., dissociative identity disorder); neurodevelopmental disorders (e.g., autism spectrum disorder); learning disorders (e.g., dyslexia, dyscalculia); and mood disorders (e.g., mood swings, irritability).
Mental health in Nigeria
Nigeria’s mental healthcare system faces a daunting crisis, with access to quality services remaining an elusive dream for many.
A severe scarcity of mental health experts, particularly in rural areas where the need is most acute, overwhelms the country’s healthcare infrastructure.
Furthermore, urban hubs largely cluster mental health services, leaving vast swathes of the country in a state of neglect, with little to no access to specialized care. Lack of integration of mental health into primary healthcare leads to a fragmented and ineffective system, further exacerbating the situation.
This perfect storm of challenges denies countless individuals the support they need, perpetuating a cycle of suffering and neglect that urgently demands attention and action.
The far-reaching consequences of untreated mental health conditions reverberate throughout entire ecosystems, affecting not only individuals but also their loved ones, communities, and society as a whole.
Unaddressed mental health challenges often lead to devastating ripple effects, such as diminished productivity, fractured relationships, and a significantly reduced quality of life.
Financial hardship, emotional exhaustion, and social seclusion may thrust families into a vortex, while societal issues such as criminal behaviour, substance abuse, and homelessness surge in communities, further straining already limited resources.
The cumulative effect It is a staggering burden that underscores the urgent need for comprehensive mental health support, not just for individual well-being but also for the collective prosperity of our communities.
Drugs as a coping mechanism
Individuals struggling with mental health concerns often turn to substance use as a coping mechanism to temporarily escape the overwhelming emotions and tension.
The drugs provide a fleeting sense of relief, offering a brief respite from their troubles and a momentary distraction from the chaos that clouds their minds.
However, this short-lived solace can lead to a vicious cycle of dependence, masking the underlying issues rather than addressing the root causes of their distress.
In June 2024, the National Drug Law Enforcement Agency (NDLEA) raised concerns about the surge in drug abuse cases in Nigeria.
The agency seized drugs worth over N40 billion in just a few weeks and warned that drug abuse has reached a critical level, threatening the nation’s well-being and requiring a collective effort to combat it.
The agency emphasizes that drug abuse has become a pervasive and alarming issue, transcending socio-economic boundaries and geographical regions.
According to NDLEA, the menace is no longer limited to vulnerable segments of society; it is also prevalent among high-profile individuals and influential personalities.
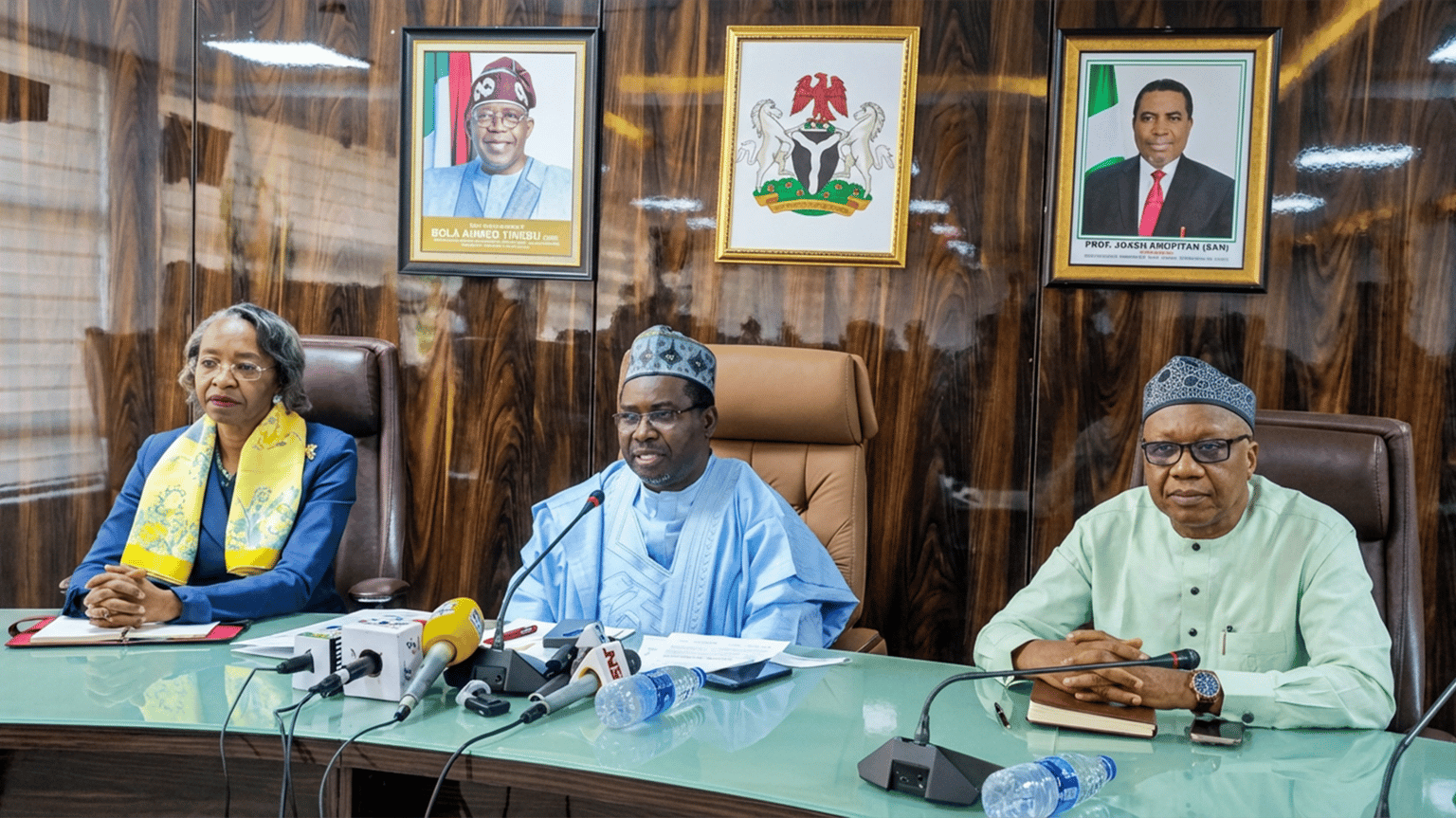
Ibinabo Archie-Abia, Assistant Commander General of Narcotics at NDLEA’s Directorate of Operations and Investigation, appeared as a guest on Arise TV’s Morning Show, offering her expert perspective and expressing her concerns about the alarming drug abuse epidemic sweeping across the nation.
Self-harm as a compensatory mechanism
Some individuals may tragically turn to self-harm as a coping mechanism, inflicting physical pain upon themselves by intentionally cutting or injuring their bodies with sharp objects, such as razor blades, in an attempt to temporarily escape the emotional anguish and distress that they may be experiencing.
This dangerous and harmful behaviour can have severe physical and emotional consequences, including infection, scarring, and worsening mental health struggles.
Suicide as a final solution
Tragically, some individuals struggling with mental health issues may feel overwhelmed by their emotional pain and succumb to the allure of suicide in a desperate attempt to escape their unbearable suffering.
In a heart-wrenching bid to find solace, they may surrender to the persistent whispers of hopelessness, allowing the darkness to consume them.
This devastating outcome is often the culmination of a long and arduous battle with inner demons, as the individual becomes exhausted from fighting to find a glimmer of hope in a world that seems devoid of light and understanding.
Dr. Titilayo Tade, Deputy Director of Medical Social Services at Lagos University Teaching Hospital (LUTH) and training coordinator for the Suicide Research and Prevention Initiative (SUPRIN), reported that the suicide rate in Nigeria was 6.9 per 100,000 people in 2019, indicating an increase from 6.5 in 2012.
However, these figures are likely underreported or miscoded, suggesting the actual rate may be even higher.
The WHO reports that Nigeria’s suicide rate is currently 9.5 per 100,000 people, one of the highest in Africa.
Section 327 of the Criminal Code Act currently criminalizes suicide in Nigeria and carries a sentence of up to one year in prison.
Additionally, Section 326 of the same act imposes a felony charge and life imprisonment for individuals who assist or encourage others to take their own lives.
However, in a recent development, the House of Representatives has proposed an amendment to replace the one-year jail term with community service and counselling as an alternative punishment for attempted suicide, marking a shift towards a more compassionate approach.
Mental health facilities in Nigeria
Across various regions in Nigeria, a network of psychiatric hospitals delivers essential mental health care to a wide range of communities, including the Neuro-Psychiatric Hospital in Aro, Abeokuta, the Federal Neuro-Psychiatric Centre in Kwara, and the Federal Neuro-Psychiatric Hospital in Uselu, Benin.
The list also includes additional facilities, such as the Federal Psychiatric Hospital in Calabar, the Federal Neuro-Psychiatric Hospital in Enugu, the Federal Neuro-Psychiatric Hospital in Kaduna, and the Federal Neuro-Psychiatric Hospital in Maiduguri.
Additional psychiatric hospitals include the State Neuro-Psychiatric Hospital in Awka, Anambra, the Psychiatric Hospital in Eket, Akwa Ibom, the Psychiatric Hospital in Sokoto, the Kano State Psychiatric Hospital in Kano, and the Psychiatric Hospital in Abia, as well as numerous other facilities that provide vital mental health services across the country.
Mental health laws in Nigeria
Nigeria’s first mental health legislation was the Lunacy Ordinance of 1916, followed by the Lunacy Act of 1958, which empowered medical professionals and magistrates to detain individuals with mental illnesses.
In 1991, Nigeria formulated its mental health policy for the first time. President Muhammadu Buhari signed the Mental Health Bill into law in January 2023, replacing the term “lunatic” with “mental health” and shifting the focus to community-based care.
The new law also established the Department of Mental Health Services in the Federal Ministry of Health, protected the rights of individuals with mental health issues, and created the Mental Health Fund to support implementation.
Stakeholders’ perspectives
Speaking on mental health issues in Nigeria, a consultant psychiatrist, Dr. Caleb Abalis, said that throughout his extensive years of practice, he has consistently encountered a range of prevalent mental health challenges that profoundly impact individuals and communities.
He said: “These common issues include substance use disorders that entrap individuals in cycles of addiction, anxiety disorders that foster relentless worry and fear, and depressive disorders that shroud lives in darkness and hopelessness.
“Schizophrenia distorts reality and disrupts thought processes, while organic mental disorders such as seizure disorders alter brain function and impair daily life.”
“These complex conditions necessitate compassionate understanding, expert care, and supportive interventions to facilitate healing and recovery.
According to Dr. Abalis, people attribute mental disorders to certain cultural beliefs and therefore do not approach Orthodox mental health care until things have seriously deteriorated.
He said: “Mental illness is often shrouded in shame due to cultural misconceptions and stigmatizing beliefs, leading to secrecy and delayed treatment. Even when individuals decide to seek help, cultural norms can hinder timely care, as family decision-makers may prioritize traditional values over medical intervention.
“Furthermore, the stigma surrounding mental health treatment deters many from adhering to medication regimens, fearing judgment and exposure by being seen at mental health facilities, thereby exacerbating the suffering and prolonging recovery.
According to Abalis, individuals can access comprehensive mental health resources and support through a multifaceted network of channels, encompassing dedicated mental health departments within teaching hospitals, specialist hospitals, and general hospitals.
He said: “Additionally, standalone psychiatric hospitals and specialized private hospitals offer mental health care services.Non-governmental organizations also provide vital support, complemented by family and social support systems. Furthermore, religious organizations offer spiritual guidance and resources to support mental wellbeing.”
Abalis emphasized that the path to mental wellness commences with a vital acknowledgement: understanding that mental illness is a genuine medical condition, deserving of compassion and treatment rather than a reflection of personal weakness or moral deficiency.
He said: “This fundamental awareness determines whether individuals will seek help in the first place. However, even when they do, a second hurdle emerges: the scarcity of mental health resources and expertise within hospitals.
“Furthermore, the crushing weight of stigma—both societal and institutional—threats to silence those who need help the most, and finally, poverty’s suffocating grip can render even the most well-intentioned treatment plans unattainable.’’
To combat these formidable obstacles, Abalis said: “We must launch a multi-pronged assault: a mass media campaign to shatter stigmas and normalize mental health conversations. Grassroots community outreach to educate and empower; and the swift implementation of mental health legislation that protects patients’ rights and dignity.
“By subsidizing or providing free treatment, we can ensure that financial constraints no longer stand in the way of healing and recovery. Awareness and education efforts should be sustained and ongoing, with regular initiatives and programmes that foster a continuous dialogue about mental health.
“To truly resonate with the community, it’s essential to engage and empower community leaders, members, and, most importantly, individuals living with mental illness, as their personal experiences and insights are invaluable. By doing so, we can create a supportive ecosystem that encourages open conversations, dispels stigmas, and promotes inclusivity.”
The consultant said that a collaborative approach will not only raise awareness but also ensure that the voices of those affected are heard, valued, and integral to the solution.
He believes that rural health centres should have access to a wide range of free or subsidized medications to combat mental illness and that health workers should receive thorough training to confidently diagnose and treat mental health conditions.
He said: “Moreover, mentorship programmes can be established, where seasoned mental health professionals embark on regular visits to rural areas, sharing their expertise and guiding local health workers in providing top-notch care.
“Furthermore, families who steadfastly support their loved ones on the journey to mental wellness should be recognized and rewarded with incentives, acknowledging the vital role they play in fostering a supportive environment that nurtures recovery.”
Association of Psychiatrists in Nigeria’s (APN) reaction
In a recent interview, Prof. Taiwo Obindo, President of the Association of Psychiatrists in Nigeria (APN), lamented the glaring disparity in the country’s mental healthcare system, revealing that Nigeria falls woefully short of the recommended ratio of one psychiatrist to 10,000 people.
The country’s meagre workforce of less than 250 psychiatrists struggles to meet the burgeoning mental health needs of its citizens due to its staggering population of over 216 million.
To put this into perspective, the population’s mental health needs require at least 21,600 psychiatrists.
The United Nations Department of Economic and Social Affairs’ dire statistics, according to Obindo, paint a grim picture: a single psychiatrist must provide care for a staggering 864,000 Nigerians.
He emphasized that the mental health policy mandates a robust and comprehensive approach, requiring every federal medical centre, general hospital, and specialist centre to establish a dedicated mental health department or, at the very least, a specialized unit.
Furthermore, the policy vision prioritizes and holistically addresses mental wellbeing alongside physical health by calling for the seamless integration of mental health services into primary healthcare.
He said the stark reality is that numerous general hospitals beyond Lagos State’s borders are woefully ill-equipped to address mental health concerns, with psychiatrists and clinical psychologists glaringly absent.
This devastating shortage leaves countless individuals struggling with mental health issues in a state of utter despair, devoid of access to the vital care they so desperately need.
According to Obindo, the disproportionate concentration of mental health facilities in urban hubs forces rural residents to travel long distances in a desperate attempt to receive the necessary treatment.
Stories of Survivors and Advocates
Ms. Hauwa Bitrus, a courageous mental health advocate, has bravely battled obsessive-compulsive disorder (OCD) for as long as she can remember. Her unwavering resilience and determination inspire hope and strength in others facing similar struggles.
Hauwa revealed that a crippling fear of germs and a relentless pursuit of cleanliness constantly plague her with an overwhelming compulsion to repeat certain actions multiple times.
She described how she obsessively scrutinizes her hands, scrutinising every detail with intense anxiety, and how she feels an unrelenting need to clean her home repeatedly throughout the day, perpetually striving for an unattainable standard of perfection.
Hauwa poignantly recalled how her family, despite noticing her struggles, failed to comprehend the depth of her suffering, with her parents acknowledging something was amiss but downplaying its significance.
Her siblings, however, misinterpreted her repetitive behaviours as a ploy to seek praise, unaware of the turmoil that drove her actions.
Meanwhile, her classmates in primary and secondary school would mockingly label her a “perfectionist” and “eye service” expert, cruelly trivializing her struggles with OCD.
Hauwa’s voice cracked with emotion as she revealed how the debilitating grip of OCD had ravaged her social life, leaving her feeling like a social outcast.
She recounted how her peers would taunt her, attributing her peculiar behaviours to the sinister influence of an “Ogbanje spirit,” a malevolent entity in Nigerian folklore.
The weight of their misinformed perceptions and judgments isolated her, making it difficult for her to form meaningful connections or find solace in friendships.
“The disorder wreaked havoc on my life, breeding uncertainty and self-doubt as I grappled with the scant knowledge available at the time,” she recounted.
“Though my loving parents offered unwavering support, their lack of understanding only added to my distress. My siblings, unfortunately, were far from empathetic; their youthful insensitivity only exacerbated my struggles. However, with time and maturity, they came to realize the gravity of my struggles, and their support finally arrived.
“My siblings would often accuse me of repeating household chores just to seek our parents’ attention, like re-sweeping a room that had already been swept by them. I vividly remember a particular incident where I re-washed clothes that my younger sister had already washed, convinced that they weren’t clean enough, despite their obvious cleanliness.
“A retired nurse, who had returned from Ghana and lived in our community, played a pivotal role in my journey. She was the first person to identify my struggles as OCD and took the time to educate me about the condition, offering valuable guidance on how to cope with the overwhelming urge to repeat tasks.
“This was an era before readily available internet access and Google searches, so her insight was truly a beacon of hope in my darkest days. I am overjoyed to witness mental health issues finally receiving the long-overdue attention they so desperately require.
“It’s a significant step forward, but I implore the government to take it a step further by launching comprehensive public awareness campaigns that demystify mental health and its complexities.
“By collaborating with mental health advocacy groups, they can develop innovative solutions to support the courageous individuals fighting these battles, ultimately fostering a society that prioritizes emotional well-being and provides a supportive ecosystem for mental health warriors to thrive.”
Mrs. Fiberesima Udom, a caregiver for a dementia patient, emphasized that caring for someone with dementia is an incredibly challenging and exhausting experience.
She highlighted that while dementia significantly impacts an individual’s mental health, it is essential to understand that dementia itself is not a mental illness but rather a condition that affects memory, thinking, and behaviour.
Despite this distinction, it is impossible to overstate the emotional toll on both caregivers and patients.
She said: “My mother has been battling dementia for almost 12 years, and it’s been a difficult journey for me and our family.”
Fiberesima shared that one of the most heartbreaking experiences is when a loved one no longer recognizes you, and she wishes no one, not even her greatest enemy, to suffer from this debilitating disease.
She explained: “I have to repeatedly remind my mother that I’m her daughter, as she struggles to recall our relationship. Some days, she becomes agitated, accusing me of kidnapping her and denying any knowledge of who I am.
“On other days, she calmly asks me questions about her own identity, seeking information about her name, her past, her marital status, and the number of children she has. Even the strongest person can be emotionally shattered by such experiences.
“I would often find a quiet spot and cry my heart out, watching my once-strong and stubborn mother now behave like a toddler, asking childlike questions and relying on me for everything. I’m not sure how to tackle this complex issue, but I firmly believe that the government has a vital role to play in supporting individuals and families affected by dementia.
“Providing free health insurance would be a wonderful starting point, offering a beacon of hope and financial relief to those navigating this heart-wrenching journey. By doing so, we can ensure that these brave individuals receive the comprehensive care they deserve without the added burden of exorbitant medical expenses.”
Mrs. Wasalat Ibitoye bravely shared her terrifying experience, revealing that a crippling bout of postpartum depression followed the birth of her last child.
She poignantly described how the once-joyful experience of motherhood suddenly felt drained of purpose, leaving her feeling lost and disconnected from her newborn.
The task of caring for her baby, once an anticipated delight, became a daunting challenge that seemed insurmountable as the darkness of depression threatened to consume her.
She recounted how, in the immediate aftermath of birthing her precious baby, a profound sense of emptiness and hopelessness engulfed her, stripping her of her will to live.
The crushing weight of depression threatened to consume her entirely, reducing the once-vibrant spark within her to a faint flicker.
Even the most basic tasks, like caring for her newborn and breastfeeding, became Herculean challenges that felt like insurmountable battles.
Yet, in the darkest of moments, her loving husband emerged as a beacon of hope, selflessly shouldering the responsibilities of childcare and providing a lifeline of support.
She said: “For a full six months, I was a mere shadow of my former self, struggling to perform even the simplest tasks, like eating. I felt perpetually lost and disconnected from reality. My son is now a vibrant 12-year-old, full of life and energy.As I reflect on my journey, I always advise young women to choose a partner who truly loves and values them rather than settle for anyone.
“If my husband hadn’t been my rock during my darkest moments of depression, I shudder to think what might have become of me. His unwavering support and love were my lifeline, and I’m eternally grateful. Or if he gave in to suggestions to take me to a prayer house or native doctor house, I might be raving fully mad now.”
Conclusion
It is imperative that the executive branch of government take decisive action to address the mental health crisis by significantly increasing the number of psychiatrist doctors in the public sector, allocating substantial funds for mental health initiatives, and prioritizing comprehensive mental health care.
Lawmakers also have a critical role to play in championing the cause and passing legislation that safeguards the rights and dignity of mental health patients, protecting them from stigmatization, discrimination, and victimization.
We cannot overstate the seriousness of mental health issues, and it is our duty to face this reality with compassion and understanding.
By engaging in open and honest discussions, we can work to dismantle the barriers that prevent individuals from seeking help. By cultivating a culture of empathy and support, we can create a safe space for those struggling with mental health issues to come forward, share their stories, and receive the care and resources they deserve.
Denial, often rooted in fear of judgment or rejection, is a formidable obstacle to mental wellness. Anyone going through this must cultivate the confidence to voice their struggles, confide in trusted family and friends, and don’t hesitate to reach out for support when the darkness of depression threatens to consume them.
We should remember to nurture our mental harmony, fostering a state of inner peace and balance that enables people to approach life’s obstacles with clarity, confidence, and creativity, as we pursue financial stability and security






















Leave a comment